
Hi everyone, in keeping with last week’s theme on antifragility amidst the global COVID-19 crisis, this week we’re going to talk about a specific example of an antifragile system that’s probably on a lot of your minds right now: your immune system. If you have a biology background you may already know all of this, but I’m guessing most people who read this newsletter don’t. So I hope you enjoy and learn something from this quick overview on how your immune system works, and why it’s such a great example of an antifragile system that gains from disorder.
The immune system: three lines of defence
What are we talking about when we say “The immune system?” First of all, you don’t have one immune system, so much as you have three layers of defence who work to protect you from pathogens and disease. They all work together, particularly the second and third layers who coordinate their work a lot. Still, we can still think of them as three distinct systems that have their own strengths and weaknesses.
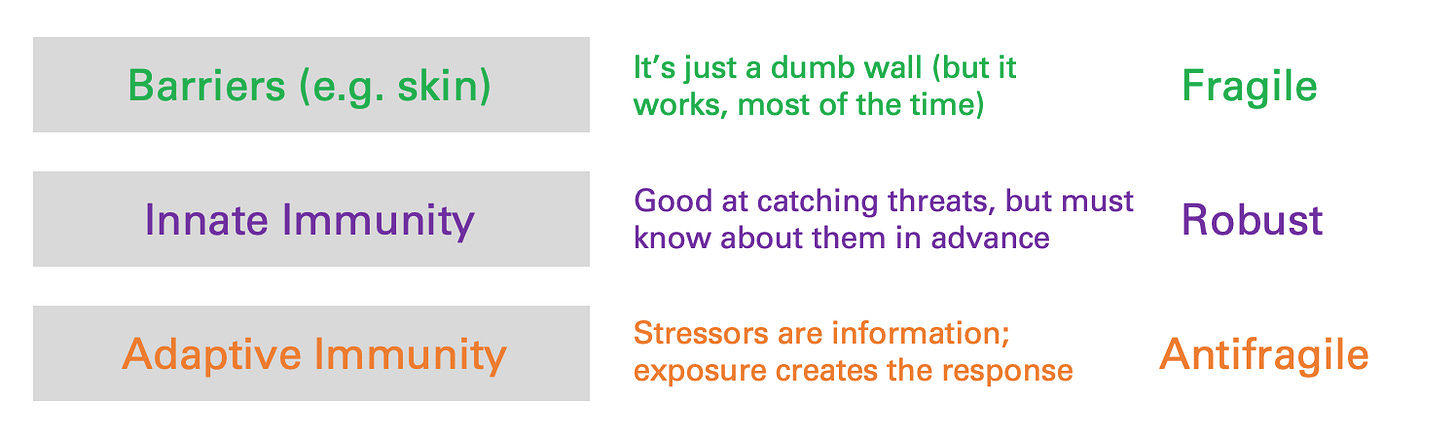
The first one is pretty easy to understand: it’s your skin. Your skin is a wall that keeps stuff out. It’s simple, but effective! It’s fragile, though. Your skin suffers when stressed. If you’ve ever had a cut that got infected, that’s what happened: the wall got breached, and you suffered the consequences. Nonetheless, it’s a good thing you have it. It’s a simple, cheap, and effective way to keep 99% of the pathogens and toxins you encounter in the world out of your body and away from where they can cause problems.
What about threats that get through the wall? The next two layers of defence are more targeted and deliberate. In vertebrate animals like us, there are two levels to our immune response: innate immunity, which is a characteristically robust system, and adaptive immunity, which is antifragile.
When you’re dealing with a threat, the immune system has to do two things: identify it, and destroy it. Destroying it, relatively speaking, is the easy part. Both the innate and adaptive immune system rely on similar weaponry to do so: we enlist specialized white blood cells and marker molecules to tag threats, break them apart, neutralize them, or just eat them. The harder part is knowing what to destroy: how does the body equip itself to know what a threat looks like, so that if it sees something, it can say something?
The innate immune system has learned what threats look like by an old, slow, but tried-and-true method: evolution. The innate immune system acquires its threat models through evolutionary selection from generation to generation, which is very slow in the context of our own lives (evolution typically takes thousands of generations to work) but still totally works as a way of identifying pathogens that have been around long before we were.
White blood cells in the innate immune system all carry around an “most wanted list” of threat models in their DNA. Remember, your DNA is more or less fixed from birth: the set you get from your parents is the set you’ve got for life, and you benefit from the evolutionary experience of thousands of generations before you. It’s spread out among every white blood cell and every precursor cell of your body, and the response that it triggers gets carried out by dozens of different cell types and attack mechanisms, so it’s pretty resilient to shock and distress.
But it only works if that threat can be identified in advance; and unfortunately “in advance” means in evolutionary terms: “before humans”. Fortunately, just as your skin is good at keeping out 99% of all bad stuff, the innate immune system is good at keeping out the next 99% of bad stuff - most pathogens that can hurt you have existed in the world for a very long time. But not all of them. So then what?
The adaptive immune system: stressors are information
In contrast to innate immunity, your adaptive immune system does not have the luxury of keeping a most wanted list handy. Your adaptive immune system has a harder job. It has to identify pathogens and bad stuff that you’ve never seen before, and possibly that no one has ever seen before. Bacteria and viruses evolve at a rate that’s orders of magnitude faster than us. We are perpetually playing catch-up in the fight against new viruses and new bacteria that have evolved into existence.

It’s worth taking a minute to go through the biological mechanics of this challenge. The way that your white blood cells detect foreign intruders is by continually testing everything they encounter for certain identifying factors, called antigens. To do that, the cells need to express their own counterpart identifiers, called antibodies and antigen receptors, which selectively bind to a specific antigen partner.
Antigen receptors, like most of the rest of the stuff in your body, are proteins; and the recipe for how to make them is in your DNA. Your innate immune system comes with its DNA recipes for antigen receptors pre-installed; you inherited them from your parents, who got it from their parents. Over time, you can evolve the right DNA recipes for catching the usual suspect pathogens. But how do you predictively design and generate antigen receptors, for threats you’ve never seen?
The adaptive immune system does something pretty remarkable here: it generates them randomly. New white blood cells repeatedly scramble and rearrange the basic building blocks of these receptors in order to generate new combinations: up to 2.25 x 10^18 potential combinations in humans, at least so we believe so far (it could be higher). Instead of trying to predict the future, your adaptive immune system instead just makes a little bit of everything.
The vast majority of these cells will never live out their intended purpose. They’ll float around, never finding that new theoretical virus for which they were randomly and specially generated. But every once in a while, one will find its target. (It doesn’t actually just run into it in the wild; that antigen gets “presented” by one of your innate immune system’s cells, who are actually a bit more clever than we’d given them credit for before. They may not know what they’re looking at, but they understand how to “hand over authority”, so to speak, to the adaptive system.) After going through a critical checklist to make sure you haven’t accidentally found part of yourself, the system gears up: it has its marching orders.
So you’ve found a real threat, and it merits a real response. The first thing your immune system does is make massive numbers of copies of that lucky white blood cell; it also powers up its own fleet of weapons that it’ll use to eliminate the threat that it now knows how to identify.
Then - and here’s the important part - once the threat is conquered, that threat is now stored permanently in our most wanted list, just like the classic threats that we automatically know how to neutralize. The next time we see that same threat, we’re ready. And we can get to work fighting it way faster; in fact so fast you never even feel sick. That’s what we mean when we say we’re immune to something, and it’s how vaccines work.
Vaccines are a clever hack. By presenting the body with a small and disabled part of a disease, we can use society’s current knowledge of what diseases are currently dangerous (which works a lot faster than evolution does) to pre-load our adaptive immune system with its own most wanted list. That’s what you’re doing when you get your shots.

In last week’s issue, one question that still seemed to trip people up a bit was the difference between optionality and antifragility. The adaptive immune system is a great illustration of the difference. The first part - pre-generating all of those randomly generated antibodies and antigen receptors - 1) is a kind of optionality, and 2) is a prerequisite for antifragility: you need to have all of these options available to you, so that you’re ready for anything.
But it’s not enough. You also have to react. The second part - using stressors as information, reacting, and establishing permanent strength because of that reaction - that’s antifragility. Or, to be fair, that’s how I use the term antifragility. It may be narrower than other definitions, but I find it’s useful to be deliberate and specific with how you use words like this.
Over the course of your life, your adaptive immune system grows stronger every time you’re exposed to new pathogens and diseases. Every time you give it a workout, it learns and strengthens. That’s why, unless you have an immune deficiency, it’s important to get a lot of exposure to dirt and germs early on when you’re young, and then continually throughout your life too.
The biggest insight here, I think, is to really wrap your head around the nature of information in this system. The presence of a new, unknown pathogen resolves uncertainty for the adaptive immune system, because it tells it something explicit: Hey, you know how you randomly generated all of those antibodies and antigen receptors? This one is the right one. The stressor tells you what to do, and then makes you stronger in a deliberate, non-accidental way.
Compare this to the innate immune system, which has no such capacity (the stressor simply goes unregistered until it’s too late) or barriers like the skin (the stressor actively makes it weaker). For the innate immune system, the stressor is not information: it does not resolve any uncertainty. Information isn’t what you’re told; it’s what you understand!
You can find a permalink to parts 1 and 2 of this post (last week + this week) here: Antifragility | alexdanco.com
If you’re looking for more non-COVID reading material this weekend, check out this very interesting piece on security by Todd Simpson.
Knights, Castles, Satchels and Writs | Todd Simpson, iNovia Capital
Many of you are probably familiar with the “Castles and Knights” metaphor of IT security; this piece extends the idea further into the present (and, I think, the future that’s beginning to arrive). Give it a read and get smarter.

And finally in the Comics Section, this week’s tweet that made me laugh the hardest:

Have a great week, and stay positive. (Attitudes; not tests!)
Alex

